Typhoid FeverWhat is typhoid and paratyphoid fever? Typhoid fever is a disease caused by the bacteria Salmonella Typhi. Paratyphoid fever is a disease caused by the bacteria Salmonella Paratyphi. These diseases cause a similar illness. Paratyphoid infections tend to be less severe and less common than typhoid. These diseases are rare in Australia and are often grouped together and called ‘enteric fever’ In Australia, most typhoid and paratyphoid infections are acquired overseas by individuals eating contaminated food or water in developing countries while visiting friends and relatives or travelling. These infections are different to infection with Salmonella which usually causes gastroenteritis. What are the symptoms? People with enteric fever may experience mild or severe symptoms. The symptoms may include:
The time from contact with the typhoid bacteria to the start of symptoms (incubation period) is usually 8-14 days but can be as early as 3 days or as late as 60 days after infection. The incubation period for paratyphoid is shorter than for typhoid, usually 1-10 days. How is it spread? The bacteria that cause typhoid and paratyphoid fever are found in the faeces of infected individuals and sometimes in their urine. Some people (known as carriers) continue to carry the bacteria even after symptoms have resolved. Transmission usually occurs when faecally-contaminated food and water are ingested. Therefore, typhoid fever is more common in less developed countries with poor sanitation, poor hand hygiene and food handling standards, and untreated drinking water. Raw fruits and vegetables and shellfish are the types of foods most often associated with illness. Flies may transfer the bacteria to food. Who is at risk? Typhoid fever is widespread in most parts of the world except for the developed regions. In Australia, enteric fever almost always occur in people who travel to areas where enteric fever is common. Immigrants who return to developing countries (in particular India, Pakistan and Bangladesh) to visit friends and relatives are at greatest risk of acquiring the disease. People who have travelled or live with an infected person will be screened for typhoid fever by their local public health unit. Household contacts, or people who have travelled with a person infected with typhoid, will be screened for typhoid by their local public health unit. Contacts should be aware of the symptoms of typhoid and should see their general practitioner if they develop symptoms. How is it prevented? People travelling to countries where typhoid and paratyphoid fever are common should:
Vaccines Typhoid vaccination is recommended for all travellers two years of age and older going to endemic regions where food hygiene may be suboptimal and drinking water may not be adequately treated. Monovalent typhoid vaccines
 Combination vaccine that contains S. Typhi & Hepatitis A
Unfortunately, there is no vaccination available for paratyphoid. People infected with typhoid or paratyphoid fever, or who share a house with someone infected with typhoid, MUST NOT work if their work involves food handling or caring for children, patients or the elderly, and should not prepare food for others until stool samples have shown that they are not infectious. A number of stool tests will be required to assess when you are no longer infected. Your local public health unit will advise you when are able to return to work. How is it diagnosed? To diagnose typhoid and paratyphoid fever, your general practitioner or local hospital will send a blood or stool sample to a laboratory for testing. How is it treated? Enteric fever is treated with antibiotics. Antibiotic treatment is required to treat carriers also. If symptoms are severe, hospitalisation may be needed. What is the public health response? Doctors, hospitals and laboratories must notify cases of typhoid or paratyphoid fever to the local public health unit. Public health unit staff will interview the doctor or patient (or carers) to find out how the infection occurred. The NSW Food Authority, in collaboration with NSW Health, is responsible for the environmental investigation of food handlers with typhoid or paratyphoid fever. Your local public health unit can advise further regarding exclusions from work and school. People excluded from work will need to have a number of stool tests done before they are allowed to return to work. For further information please call your local Public Health Unit on 1300 066 055 Typhoid fever is a systemic infection caused by Salmonella Typhi, usually through ingestion of contaminated food or water. The acute illness is characterized by prolonged fever, headache, nausea, loss of appetite, and constipation or sometimes diarrhoea. Symptoms are often non-specific and clinically non-distinguishable from other febrile illnesses. However, clinical severity varies and severe cases may lead to serious complications or even death. It occurs predominantly in association with poor sanitation and lack of clean drinking water. According to the most recent estimates (published in 2014), approximately 21 million cases and 222000 typhoid-related deaths occur annually worldwide. 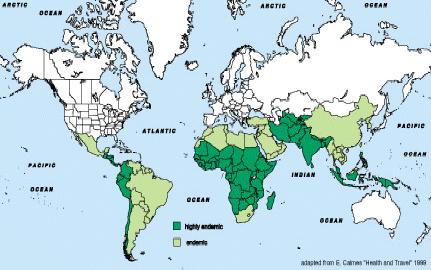 Light green: endemic - Dark green: highly endemic Two typhoid vaccines are currently recommended for use by:
WHO recommends the use of the Vi-PS and Ty21a vaccines to control endemic disease and for outbreak control. WHO further recommends that all typhoid fever vaccination programmes should be implemented in the context of other efforts to control the disease, including health education, water quality and sanitation improvements, and training of health professionals in diagnosis and treatment. Several Vi polysaccharide–protein conjugate vaccine candidates are under development (or are nationally licensed but not on the international market) and anticipated to be available in the future for infant immunization. Source: World Health Organisation |
|
Covid-19 Notices
Flu Shot Emergency Numbers After Hours 13 74 25 Contact Hours |
Doctors
Appointments Fees About Map Links |
Immunisation
Feedback Local Pharmacies Resources Home |
| 
|

| 
| 
| 
| 
|
|---|---|---|---|---|

| 
| 
| 
| 
|



